Cancer—a word that often strikes fear—is frequently discussed as if it’s something that can be cured as quickly as we produced the Covid-19 vaccine. However, cancer is not a single disease but a collection of related diseases, each with its own complexities. It is a silent plague that affects all of us in one way or another. While often perceived as a modern affliction, its strain on human physiology has been present since humans first walked the earth. Its relentless growth fills us with more cells than we need, ultimately disrupting organ function and making us the ultimate Darwinian subjects.
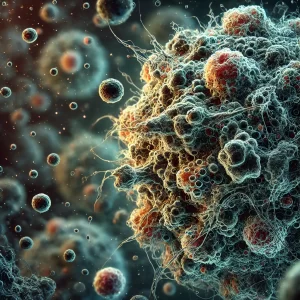
Reading Siddhartha Mukherjee’s The Emperor of All Maladies raises a poignant question. Cancer, in its purest form, is a rogue cell—traumatised, altered by disease, lifestyle choices, and aging. It’s in us—cancer. It’s a mutation of what is already there. In this twisted way, cancer is a cell that has something wrong with it and just needs fixing. We try to manage it, yet it continues to divide and reproduce, much like humans who are fundamentally designed to procreate rather than live extended lives. The older we get, the propensity to get cancer increases. And yet, we look to doctors for the answers, hoping they will fix us.
Let me tell you something: I’ve worked with them. Trust me, as amazing as these guys are, they can’t fix everything. Sometimes, you just have to die.
But you have a superpower—your immune system.
It’s thought that throughout our lives, we develop cancers all the time, and the immune system deals with it. But the older you get, the weaker that immune system is. Its ability to protect you gets as tired as you do trying to get out of bed in the morning. Your immune system wanes like a fading sun on a distant horizon, one minute it’s there, casting all sorts of bright colours, and then suddenly, it disappears. The metaphor strikes so many chords in this conversation.
But let’s cast the net further back.
Cancer is not a modern affliction. Some of the earliest mentions of cancer can be found in the Edwin Smith Papyrus dating back to 3000 BC. It describes breast tumours treated with cauterisation, noting there was no treatment for the disease. Fossilised mummies from the same era have shown signs of osteosarcoma.
Hippocrates, the Greek physician often called the ‘Father of Medicine,’ used the terms karkinos and karkinoma to describe tumours, likening them to crabs due to their appearance. The use of karkinos, meaning crab, was inspired by the disease’s appearance, with tumours often having a central mass with extending branches, resembling a crab’s shape. Additionally, the hard, invasive nature of some tumours might have reminded early physicians of a crab’s claws. This metaphorical naming reflects an attempt to understand and categorise the disease based on its physical characteristics. The term evolved into carcinoma in Latin, which is still used in modern medical terminology to describe malignant tumours, particularly those that arise from epithelial cells. Even Galen, another influential Greek physician, wrote about tumours, advocating primitive surgery and acknowledging that some cancers were untreatable.
The term Onkos is an ancient Greek word that primarily means ‘mass’ or ‘burden.’ In the context of medicine, it refers to swelling or tumours. The ancient Greeks used this term to describe any kind of mass or lump, which could be a benign or malignant tumour. The word has persisted in modern medical terminology as part of oncology, the branch of medicine that deals with tumours and cancer. This reflects the ancient understanding of abnormal growths in the body, recognising their physical presence as a burden or weight.
Both Onkos and Karkinos highlight the ancient Greeks’ attempts to understand and describe abnormal growths in the body. These terms laid the groundwork for the medical language we use today to discuss and treat cancer. Understanding these historical roots offers insight into the long-standing human struggle to comprehend and combat this pervasive disease.
Modern understanding of cancer has been greatly enhanced by research into telomeres, the protective caps at the ends of chromosomes. Telomeres shorten with each cell division, and when they become too short, cells enter a state called senescence or undergo apoptosis (cell death). This process is part of the natural aging mechanism but also acts as a tumour suppressor. However, cancer cells often evade this by activating an enzyme called telomerase, which maintains telomere length and allows the cells to continue dividing uncontrollably. Telomere shortening and the activation of telomerase are crucial factors in the development of many cancers, particularly as people age. While shorter telomeres can limit cellular proliferation, they also increase the risk of genomic instability, potentially leading to cancer. In most human cancers,
telomerase is reactivated, helping the cancer cells avoid senescence and become ‘immortal’.
With the advent of systematic record-keeping and epidemiological processes in the 18th century, it became evident that cancer primarily affected the older population. Improvements in health and safety, particularly in the workplace, have undoubtedly contributed to the longevity of people, and consequently, the higher prevalence of cancer among older individuals.
Ultimately, why are we striving to cure cancer? What drives us to combat a disease that has been silently afflicting humanity for thousands of years? Genetic growth and malignant growth are intrinsically linked. While we may manage to stop the disease by surgically removing tumours or irradiating cancerous cells, curing cancer is beyond the reach of modern medicine. The belief that cancer can be completely cured is somewhat presumptuous. Charities often assert that donations can lead to a cure, but while cancer research is crucial for halting or slowing its progression, the notion that we can eradicate this ancient malady is akin to chasing an illusion.
Rudolf Virchow, born in 1821, was a pioneering figure in medicine and pathology. He revolutionised medical science with his cell theory, famously stating Omnis cellula e cellula (All cells come from cells), and developed the concept of Virchow’s triad to explain blood clot formation. Beyond his scientific contributions, Virchow was a passionate advocate for public health and social reform, recognising the critical link between socio-economic conditions and health. He served in the German Parliament, championing progressive causes and striving for social justice. Virchow’s work extended to anthropology and archaeology, where he made significant contributions. His legacy endures in modern medical practices, public health policies, and the pursuit of health equity and social justice.
Cancer has been with us for as long as humans have occupied this earth, silently shaping human history. Ancient texts and fossil records reveal that humans have battled this insidious disease for as long as we’ve existed.
While our understanding and treatment of cancer have advanced significantly, it remains a fundamental challenge, intertwined with the very essence of cellular life and aging. The development of telomere research and the discovery of telomerase, the enzyme that allows cancer cells to evade death and continue dividing, have provided critical insights into why cancer is so difficult to eradicate. Despite these advancements, cancer cells’ ability to mutate and adapt makes finding a cure an elusive goal. Modern medicine can often manage and treat cancer, prolonging life and improving quality of life, but curing it entirely remains out of reach.
The drive to cure cancer is fuelled by a mix of hope, scientific curiosity, and the desire to alleviate suffering. However, we must recognise that while we can make strides in treatment and prevention, the complete eradication of cancer might be an unrealistic expectation. Charities and research organisations play a vital role in funding important research, but the promise of a cure can sometimes be overly optimistic.
As we walk this earth, we will walk hand in hand with the leveller that is cancer. It is a reminder of our mortality and the delicate balance of life. Embracing this reality doesn’t mean giving up the fight; it means focusing on understanding cancer better, improving treatments, and enhancing the quality of life for those affected. In doing so, we honour the countless lives touched by this ancient disease and continue the quest for knowledge and compassion in our approach to healthcare.
Cancer has become more prevalent because of advancements in medical technology, vaccine therapy, good hygiene, health and safety in the workplace, and better sanitary conditions and cleaner water. The knock-on effect of this better understanding changed the face of diseases that once blighted countries. Tuberculosis, polio, scurvy, and pellagra have dwindled, allowing cancer to come to the forefront. It hadn’t got worse or better, just more prevalent. It was just there, but shouting louder as other diseases dropped off.
If genetically, you drew the short straw of life, you got cancer. If you smoked, your propensity to get cancer increased. If you were obese, it was likely you would get cancer. If your workplace was dangerous, your chances of developing something insidious were probable. If you were lower on the socio-economic scale, you were likely to die earlier because of cancer.
And statistically, this hasn’t changed. We only have to look at the Black Report conducted by Douglas Black in the UK to realise a lot of things haven’t changed, particularly for the less fortunate socio-economic demographic.
A third voice in the cancer life cycle became louder in the 1980s. As chemotherapy failed, patients were left out in the cold, just to die. The word ‘palliative’ was born. Nothing had changed in the concept of care with cancer. For millennia, people cared for the elderly and the sick, the sick being one of the regulars such as TB, etcetera. But cancer too.
In the sphere of medicine, when the drugs don’t work, people still need to be cared for. The term ‘palliative care’—palliative is Latin for ‘cloak’—was introduced. Providing pain relief to cloak the illness, smothering the symptoms, and making the patient comfortable became the focus. This isn’t denial. When all else has failed, we must still care for these unfortunates. The use of opiates such as morphine and fentanyl are used liberally with cancer patients who have been palliated. To relieve the pain they are suffering, to quell the sense of anxiety and allow them to die with some dignity.
Cancer has not only persisted through the ages but has also evolved with our understanding of disease and treatment. As we’ve conquered other maladies, cancer has become more prominent in our collective consciousness. The prevalence of cancer is not merely a consequence of our modern lifestyle but an inevitable result of our extended lifespans and improved healthcare systems.
With better sanitation, vaccination, and overall healthcare, many diseases that once decimated populations have been controlled or eradicated. Tuberculosis, polio, scurvy, and pellagra—once common and deadly—have receded into the background, making way for cancer to take centre stage. It’s not that cancer has become more aggressive or widespread; it’s that it has become more noticeable as other diseases have been mitigated.
Genetic predisposition, lifestyle choices, and environmental factors play significant roles in the development of cancer. Drawing the genetic short straw means a higher likelihood of developing cancer. Smoking, obesity, and exposure to carcinogens increase the risk. Socio-economic status also impacts cancer outcomes, with those in lower economic brackets often facing higher risks and poorer outcomes due to lack of access to healthcare and preventive measures.
The Black Report highlighted these disparities, showing that despite advancements in medicine, socio-economic factors still heavily influence health outcomes. The report’s findings remain relevant today, underscoring the need for equitable healthcare access and social reforms to address these persistent inequalities.
The concept of palliative care emerged in response to the limitations of curative treatments. When chemotherapy and other aggressive treatments fail, the focus shifts to comfort and quality of life. Palliative care, derived from the Latin word for ‘cloak,’ aims to shield patients from the harsh realities of their illness by managing pain and symptoms, thus allowing them to live their remaining days with dignity and as little suffering as possible.
By embracing the reality of cancer and its complexities, we can better navigate the delicate balance between life and death. This approach allows us to honour the lives touched by cancer and continue the quest for knowledge, compassion, and equity in healthcare. In doing so, we move towards a future where cancer is not just a disease to be feared but a condition to be managed with dignity, understanding, and hope.